Your Guide to Discussing Breast Reconstruction with Your Plastic Surgeon

Facing a mastectomy or lumpectomy due to breast cancer or other medical conditions is daunting. Yet, the decision-making doesn’t end there. Breast reconstruction after mastectomy is a pivotal aspect of the healing journey for many women.
This article guides you through the process of meeting with your plastic surgeon to discuss breast reconstruction options.
Understanding Your Choices
Embarking on the journey of breast reconstruction begins with understanding the array of choices available. By acquainting yourself with these options, you equip yourself with knowledge that can help facilitate a more informed and meaningful discussion with your surgeon.
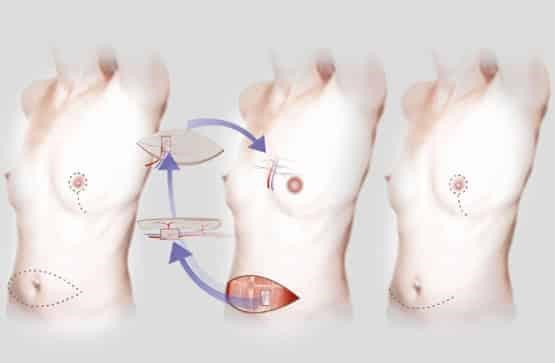
Implant-based Reconstruction
What is it?
Implant-based reconstruction involves the placement of saline or silicone gel-filled implants to recreate the breast mound. It can be done immediately after a mastectomy (immediate reconstruction) or at a later date (delayed reconstruction).
Procedure:
- Tissue Expander: Initially, a tissue expander might be placed under the chest muscle. Over weeks or months, saline solution is injected into the expander, gradually stretching the skin and making space for the implant.
- Permanent Implant: Once the skin is stretched adequately, a second surgery replaces the expander with a permanent implant.
Pros and Cons:
Pros:
- Shorter Recovery Time: Generally, implant-based reconstructions have shorter recovery times compared to autologous methods.
- No Donor Site: Since no tissue is taken from other parts of the body, there are no additional surgical sites to heal.
Cons:
- Maintenance: Implants might require replacement or adjustment surgeries in the future.
- Complications: Risks include implant rupture, rippling, or capsular contracture (scar tissue around the implant).
Autologous or Flap Reconstruction
What is it?
Flap reconstruction involves using tissue (skin, fat, and sometimes muscle) from another part of your body to create a new breast mound.
Types of Flap Reconstructions:
- TRAM (Transverse Rectus Abdominis Muscle) Flap: This method repurposes tissue from the lower abdomen.
- DIEP (Deep Inferior Epigastric Perforator) Flap: Similar to TRAM but spares the muscle, using only skin and fat.
- Latissimus Dorsi Flap: Involves tissue from the upper back.
- Gluteal Free Flap: Utilizes tissue from the buttocks.
Pros and Cons:
Pros:
- Natural Look and Feel: Since it uses your tissue, the reconstructed breast has a more natural texture.
- Long-lasting Results: No need for replacements as with implants.
Cons:
- Longer Surgery and Recovery: These procedures are more extensive and require a longer healing period.
- Donor Site Complications: There can be complications or scarring at the tissue donor site.
Combination of Implant and Flap Reconstruction
What is it?
This approach combines both flap and implant techniques to reconstruct the breast, providing both volume and a natural feel.
Pros and Cons:
Pros:
- Versatility: It can be a solution for women with limited skin availability after mastectomy.
Cons:
- Complexity: This method can combine potential complications from both implant and flap procedures.
By exploring these options and understanding their intricacies, you empower yourself to have a detailed and productive conversation with your surgeon. Recognizing the pros and cons of each method can help you align your expectations and desires with the realities of the procedures available.
Setting Your Priorities
Before your meeting, reflect on what is most important to you in terms of recovery time, appearance, feelings, scars, and long-term considerations.

Preparing for the Consultation
When meeting your plastic surgeon, preparation is key. Here are some crucial aspects:
Questions to Ask
- What are the risks and complications?
- What results can I realistically expect?
- What is the recovery period like?
- How will the reconstruction impact my daily life and activities?
- What happens if I gain or lose weight?
- How will aging affect the reconstructed breast?
Understanding Your Surgeon’s Approach
Every surgeon has a unique approach and expertise. Discussing their experience, previous results, and their suggested approach for your case can provide insight and comfort.
Visualizing Your Results
Many surgeons use 3D imaging or photographs to help you understand potential outcomes. Discuss your desires regarding size, shape, and appearance.
Understanding the Timeline
Discuss when the best time for reconstruction is, whether immediate (at the time of mastectomy) or delayed. Consider your overall treatment plan and how reconstruction fits into it.
Emotional and Psychological Aspects
Recognize that the decision is not just physical but deeply emotional. Some women find solace in regaining a semblance of their pre-surgery body, while others may choose to forego reconstruction altogether.

Financial and Logistical Considerations
Understanding costs, insurance coverage, and the logistics of recovery (time off work, support during recovery) is crucial.
The Road to Decision Making
Once armed with information, take time to weigh your options. It’s important to feel confident in your decision, knowing that it aligns with your physical and emotional well-being.
Conclusion
Choosing to undergo breast reconstruction is a multifaceted decision encompassing medical, emotional, financial, and aesthetic considerations. By engaging in open dialogues with your surgeon and reflecting on your priorities, you can navigate this path empowered and informed.
Remember, the journey is deeply personal, and the right choice is one that aligns with your unique needs and desires.